Tonsillectomy
Is the surgical removal of the tonsils, two oval-shaped pads of tissue at the back of the throat — one tonsil on each side.
A tonsillectomy was once a common procedure to treat infection and inflammation of the tonsils (tonsillitis). Today, a tonsillectomy is usually performed for sleep-disordered breathing but may still be a treatment when tonsillitis occurs frequently or doesn’t respond to other treatments.
A tonsillectomy may also be necessary to treat breathing and other problems related to enlarged tonsils and to treat rare diseases of the tonsils.
Recovery time for a tonsillectomy is usually at least 10 days to two weeks.
Why it’s done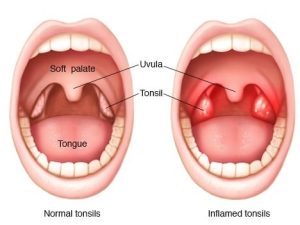
A tonsillectomy is used to treat:
- Recurring, chronic or severe tonsillitis
- Complications of enlarged tonsils
- Bleeding of the tonsils
- Other rare diseases of the tonsils
Tonsillitis
The tonsils are the immune system’s first line of defense against bacteria and viruses that enter your mouth. This function may make the tonsils particularly vulnerable to infection and inflammation. However, the tonsil’s immune system function declines after puberty — a factor that may account for the rare cases of tonsillitis in adults.
Complications of enlarged tonsils
Tonsils may become enlarged after frequent or persistent infections, or they may be naturally large. A tonsillectomy may be used to treat the following problems caused or complicated by enlarged tonsils:
- Difficulty breathing
- Disrupted breathing during sleep (obstructive sleep apnea)
Other diseases or conditions of the tonsils
A tonsillectomy may also be used to treat other rare diseases or conditions of the tonsils, such as:
- Cancerous tissue (malignancy) in one or both tonsils or suspected malignancy
- Recurrent bleeding from blood vessels near the surface of the tonsils
- Severe bad breath (halitosis) related to debris in the crevices of tonsils
Risks
Tonsillectomy, like other surgeries, has certain risks:
- Reactions to anesthetics.Medication to make you sleep during surgery often causes minor, short-term problems, such as headache, nausea, vomiting or muscle soreness. Serious, long-term problems are rare, though general anesthesia is not without the risk of death.
- Swelling of the tongue and soft roof of the mouth (soft palate) can cause breathing problems, particularly during the first few hours after the procedure.
- Bleeding during surgery.In rare cases, severe bleeding occurs during surgery and requires additional treatment and a longer hospital stay.
- Bleeding during healing.Bleeding can occur during the healing process, particularly if the scab from the wound is dislodged too soon.
- Rarely, surgery can lead to an infection that requires further treatment.
How you prepare
Information you’ll likely be asked to provide includes:
- All medications, including over-the-counter drugs and dietary supplements, taken regularly
- Personal or family history of adverse reactions to anesthetics
- Personal or family history of bleeding disorders
- Known allergy or other negative reactions to medications, such as antibiotics
Instructions for preparing will include the following:
- Your doctor may ask you to stop taking some medications or change dosages of medications several days before the surgery.
- Don’t eat anything after midnight before the scheduled surgery. Your surgeon should provide you with instructions about eating food and drinking liquids prior to reporting to the hospital.
- Make arrangements for a ride home.
- Plan for 10 days to two weeks or more of recovery time. Adults may need more time than children do.
Questions to ask your doctor or the hospital staff for yourself or on behalf of your child include:
- What are my dietary restrictions before surgery?
- When should I arrive at the hospital?
- Where do I need to check in?
- What prescription medications can I take in the days before surgery? When can I take the last dose?
- What is the expected recovery time?
- What restrictions to activities or diet should I expect during recovery?
Tests or bloodwork may be required before surgery. Your doctor may also order a sleep study (polysomnography) if a tonsillectomy is intended for treating obstructive sleep apnea, other obstructions of the airway and some other conditions.
Before the procedure
A nurse may use a pre-surgery checklist of questions, such as asking you to say your name and the reason for your surgery. This is a standard procedure to ensure the safety of patients.
During the procedure
Because a tonsillectomy is performed under general anesthesia, you or your child won’t be aware of the procedure or experience pain during the surgery.
The surgeon may cut out the tonsils using a blade (scalpel) or a specialized surgical tool that uses heat or high-energy heat or sound waves to remove or destroy tissues and stop bleeding.
After the procedure
Common issues after a tonsillectomy include the following:
- Moderate to severe pain in the throat for one to two weeks
- Pain in the ears, neck or jaw
- Nausea and vomiting for a few days
- Mild fever for several days
- Bad breath for up to two weeks
- Swelling of the tongue or throat
- Feeling of something stuck in the throat
- Anxiety or sleep disturbances in children
Steps to manage pain and promote a good recovery include the following:
- Take pain medications as directed by your surgeon or the hospital staff.
- It’s important to get plenty of fluids after surgery to avoid dehydration. Water and ice pops are good choices.
- Bland foods that are easy to swallow, such as applesauce or broth, are the best choices immediately after surgery. Foods such as ice cream and pudding can be added to the diet if they’re tolerated. Foods that are easy to chew and swallow should be added to the diet as soon as possible. Avoid acidic, spicy, hard or crunchy foods that may cause pain or bleeding.
- Bed rest is important for several days after surgery, and strenuous activities — such as running and bike riding — should be avoided for two weeks after surgery. You or your child should be able to return to work or school after resuming a normal diet, sleeping normally through the night and not needing pain medication. Talk to your doctor about any activities that should be avoided.
When to see the doctor or get emergency care
Watch for the following complications that require prompt medical care:
- You may see small specks of dark blood from the nose or in the saliva, but any bright red blood requires a trip to the emergency room for a prompt evaluation and treatment. Surgery to stop bleeding may be necessary.
- Call your doctor if you or your child has a fever of 102 F (38.9 C) or higher.
- Call your doctor if you observe signs of dehydration, such as reduced urination, thirst, weakness, headache, dizziness or lightheadedness. Common signs of dehydration in children include urinating fewer than two or three times a day or crying with no tears.
- Breathing problems.Snoring or noisy breathing is common during the first week or so of recovery. However, if you or your child is having difficulty breathing, get emergency care.